Pain in the heel is a common area of discomfort and there are many treatment options available. At this present moment in time our Podiatrists at South West Podiatry are seeing a rise in patients complaining of heel pain during Covid-19. We can offer video consultations or Face to Face consultations at this time.
What is heel pain?
Heel Pain is an umbrella term which refers to pain under the heel bone. There are approximately 40 different conditions that can affect the heel. Therefore, it should be classed as plantar heel pain until an accurate diagnosis is made by a Podiatrist or health professional.
Sometimes multiple conditions can co-exist. Plantar Fasciitis is the most common cause of foot pain in adults. The term Plantar Fasciitis is interchangeable and may also be referred to as “heel spurs” or “plantar fasciopathy”
| Other causes of Plantar Heel Pain |
| Heel fat pad inflammation, bursitis |
| Bony conditions such as a stress fracture |
| Nerve entrapments |
| Inflammatory conditions such as Rheumatoid arthritis |
| Surrounding tendon or muscle abnormalities |
| Referred pain from lumbar spine such as Sciatica |
| Neoplastic tumors or abnormal growths |
| Peripheral neuropathy and diabetes |
What are the symptoms?
- A sharp stabbing pain under the heel or arch
- Pain when rising from bed, or after a prolonged period of sitting
- Pain which is tolerable and warms up with physical activity, but worsens with fatigue and worsens after activity
What is the Cause?
When the cumulative load in the plantar fascia exceeds what the tissue can tolerate. This is often due to a combination of the following risk factors:
| Intrinsic Risk Factors | Extrinsic Risk Factors |
| Increased foot pronation (flat feet) | Training error (too much too soon) |
| Increased foot supination (high arched feet) | Inadequate footwear |
| Reduced ankle dorsiflexion (stiff ankles) | Working on hard surfaces |
| Inefficient big toe function | Prolonged standing or walking due to occupation |
| Reduced hip stability and gluteal strength | Obesity or sudden weight gain |
| Reduced foot or calf strength | Age (most common between 40-60) and menopause |
| Poor running form or other biomechanical factors | Jumping sports |
What treatments are available?
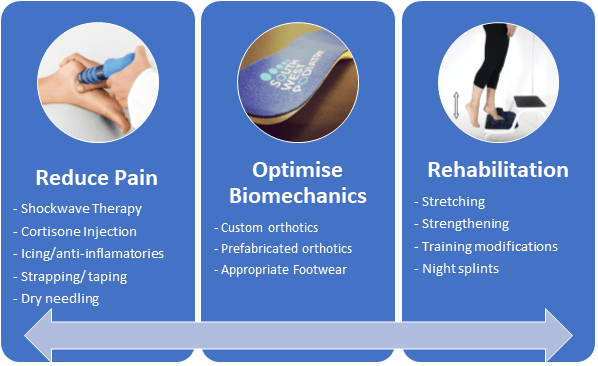
Once a diagnosis is established, a treatment plan can be made. This will ensure the quickest possible recovery and reduce the risk of future injury. Based off the duration and severity of your symptoms, plus your goals and expectations, this will typically involve a combination of the following:
Research estimates that 90-95% of patients will recover from Plantar Fasciitis with appropriate conservative treatment. However, while recovery is generally good, it can sometimes take 6-12 months for complete resolution. Surgery may be considered for patients who do not improve with conservative treatment after 12 months. This generally involves horizontal excision of the plantar fascia, and an immobilisation boot or cast is required for 4-8 weeks followed by further rehabilitation.
What should I do?
An Advanced Analysis may be booked following an initial consultation to identify the cause of mechanical stress on the plantar fascia or foot structure, caused by walking or running. An infra-red pressure assessment may also be used to provide data to analyse increased forces through your feet. Orthotics are useful for certain symptoms of plantar heel pain which are prescribed to you to improve symptoms and offload areas of the feet caused by mechanical inefficiencies.